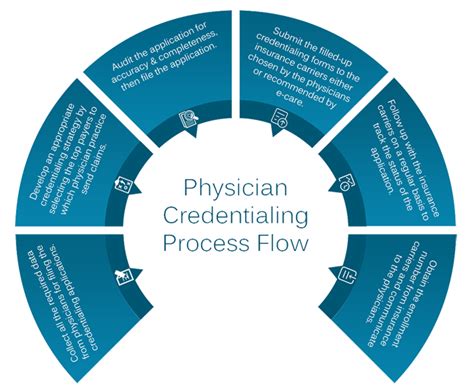
Credentialing is a process that healthcare providers must go through to ensure they meet certain standards and qualifications. The process can take a long time due to the extensive background checks and verification of credentials required. Additionally, there are often delays in obtaining necessary documentation from previous employers or educational institutions. The thoroughness of the process is necessary to ensure patient safety and quality of care.
While it may be frustrating for providers, it is important to remember that the end result is worth the wait. By ensuring that only qualified and competent providers are allowed to practice, patients can have confidence in the care they receive.
Why does it take so long to get credentialed?
The process of verifying a healthcare provider’s credentials is crucial for hospitals and health systems. This process prioritizes thorough research and accuracy, which unfortunately means that it can take anywhere from 90 to 120 days to complete. While it may not be a speedy process, it is necessary to ensure that patients receive the best possible care from qualified and competent providers.
How long does it take to get credentials?
According to the guidelines, the typical timeframe for a credentialing process is between 90 to 120 days. This process ensures that healthcare providers meet the necessary qualifications and standards to provide quality care to patients. While it may seem like a lengthy process, it is important for ensuring patient safety and the overall effectiveness of healthcare services.
How long after documents have been received does it take a carrier to credential?
“`When it comes to commercial carriers, the process of verifying credentials usually takes around 60 to 90 days. After that, the contracting phase can take an additional 30 days. This means that from the moment an insurance company receives a provider’s credentialing application, it can take a total of 90 to 120 days to complete the entire process.“`
What is checked during a credentialing process?
When applying for a medical job, there are several important pieces of information that you will need to provide. These include your education, training, and any board eligibility or certification that you have obtained. It is also important to include your work and medical staff history, as well as your clinical privilege history. Additionally, you should provide the names and email addresses of peers who can provide references for you.
By including all of this information, you can help potential employers get a better understanding of your qualifications and experience in the medical field.
What are potential consequences concerning credentialing?
Mistakes in credentialing can have serious consequences for healthcare providers and organizations. These errors can result in financial losses, delayed reimbursements, penalties, and even exclusion from government-funded programs. Additionally, patients can be put at risk due to credentialing lapses, which can lead to malpractice suits and accreditation issues. It is crucial for healthcare organizations to prioritize accurate and thorough credentialing processes to ensure the safety and well-being of both providers and patients.
Can providers see patients before payor credentialing is done?
Revised paragraph: “`Credentialing can be a lengthy process, often taking 3 to 6 months or more. Some insurance plans may also be hesitant to expand their payment exposure, making it even more challenging. One of the downsides of this process is that healthcare providers may not be able to see patients with the insurance plans until the credentialing is complete. This means that they won’t receive reimbursement for any services rendered until then.
“`
How long does it take to get credentialed through CAQH?
CAQH is responsible for verifying the accuracy and completeness of your application and accompanying documents. It usually takes CAQH between 2-5 days to approve the documents. It’s important to note that all required documents must be uploaded and approved by CAQH before your CAQH ProView profile is considered complete and accessible to HSCSN.
Can you bill Medicare if you are not credentialed?
The Medicare rule states that healthcare providers who work permanently as full-time or part-time employees must be credentialed in order to bill for Medicare services. This means that they must meet certain qualifications and standards set by Medicare in order to be eligible to receive reimbursement for the services they provide. The purpose of this rule is to ensure that Medicare beneficiaries receive high-quality care from qualified providers who meet the necessary standards of competence and professionalism. By requiring credentialing, Medicare helps to protect the health and safety of its beneficiaries and ensures that they receive the best possible care.
What is the difference between provider enrollment and credentialing?
Provider credentialing and enrollment are two important processes in the healthcare industry. Credentialing involves verifying the qualifications and suitability of a new provider for their role, while enrollment is the process of registering a provider with insurance payers so that they can receive payment for their services. Both processes are crucial for ensuring that patients receive high-quality care and that providers are properly compensated for their work. Without proper credentialing and enrollment, healthcare organizations may face legal and financial consequences, as well as damage to their reputation.
Why do most healthcare professionals require credentialing?
The process of credentialing and granting privileges is crucial in the healthcare industry. It is essential to ensure that healthcare professionals who will be delivering clinical services are qualified and competent to do so. This process involves verifying the education, training, licensure, and experience of healthcare workers. By doing so, healthcare institutions can maintain high standards of care and ensure patient safety.
Credentialing and privileges are necessary to protect patients and ensure that they receive the best possible care from qualified healthcare professionals.
What is the purpose of credentialing in healthcare?
“`Credentialing of healthcare providers is a crucial process that involves evaluating the qualifications of various types of providers. This process ensures that doctors, dentists, and other allied healthcare professionals have the necessary education, training, and licenses to provide quality care to patients. It is a vital safety measure that helps to protect patients from receiving substandard care and ensures that healthcare providers are competent and qualified to perform their duties.“`
Does credentialing refer to a certificate?
Certification, also known as credentialing, is a process where a non-governmental organization establishes standards to validate an individual’s expertise and proficiency in their respective field. It is typically a voluntary process, where an individual decides to pursue professional credentials to enhance their career prospects. This process ensures that the certified individual has the necessary knowledge and skills to perform their job effectively.
What are the 3 types of credentials?
There are various academic and occupational credentials that individuals can obtain to advance their careers. Some of the most common types include associate degrees, bachelor’s degrees, and master’s degrees. An associate degree typically takes two years to complete and provides a foundation in a specific field. A bachelor’s degree takes four years and offers a more in-depth education in a particular area of study.
A master’s degree is a graduate-level degree that requires an additional one to three years of study beyond a bachelor’s degree and provides advanced knowledge and skills in a specific field. Obtaining these credentials can lead to better job opportunities, higher salaries, and increased job satisfaction.
Is a credential better than a certificate?
Credentials are typically shorter than degrees, but they often require more general education and coursework than certificates. These certifications are issued by authorized institutions or companies and serve as evidence of your proficiency in a particular field. So, if you’re looking to demonstrate your knowledge and skills in a specific area, a credential may be the perfect option for you.
What are the elements of credentialing?
The healthcare industry relies on credentialing to ensure that healthcare providers are qualified and competent to provide care to patients. Credentialing is a thorough process that involves verifying various elements such as licensure, education, training, experience, competency, and judgment. Healthcare facilities and managed care organizations/health plans use this process to collect and verify the credentials of applicants. By doing so, they can ensure that patients receive high-quality care from qualified professionals.
What are the elements of credentialing?
The healthcare industry relies on credentialing to ensure that healthcare providers are qualified and competent to provide care to patients. Credentialing is a thorough process that involves verifying various elements such as licensure, education, training, experience, competency, and judgment. Healthcare facilities and managed care organizations/health plans use this process to collect and verify the credentials of applicants. By doing so, they can ensure that patients receive high-quality care from qualified professionals.
What is credential verification check?
Verifying the credentials of your potential employees is crucial in ensuring that they possess the necessary work experience, education qualifications, professional memberships, and trade licenses that they claim to have. This process is essential in helping your company achieve its objectives and protecting its reputation. By conducting thorough credential verifications, you can be confident that you are hiring the right people for the job and avoiding any potential legal or financial risks that may arise from hiring unqualified individuals.
What are four types of credentialing requirements that you would need to understand before beginning a job search in complementary or alternative medicine?
“`When it comes to working in certain fields, there are often requirements that must be met in order to ensure competency and safety. These requirements may include providing proof of training, obtaining licensure or certification, passing background checks, completing continuing education hours, having malpractice insurance coverage, and gaining experience in a specific setting such as a hospital or research environment. By meeting these requirements, individuals can demonstrate their qualifications and commitment to their profession, while also ensuring the safety and well-being of those they work with.“`
What are credentialing processes used in nursing?
The evaluation of healthcare professionals’ competencies and credentials, which includes registration, certification, and licensure, is known as credentialing. Patients have the right to receive top-notch nursing care, which necessitates that nurses be qualified and trained to provide services.
Related Article
- Why Does Creatine Taste So Bad?
- Why Does Creatine Make You Pee?
- Why Does Creatine Make Me Poop?
- Why Does Creatine Make Me Pee?
- Why Does Cox Need My Ssn?
- Why Does Coutu Consider Schmidt Resilient?
- Why Does Coughing Make You Higher?
- Why Does Cora Call Mr Brown?
- Why Does Cooked Crab Turn Black?
- Why Does Colbert Say Is Potato?